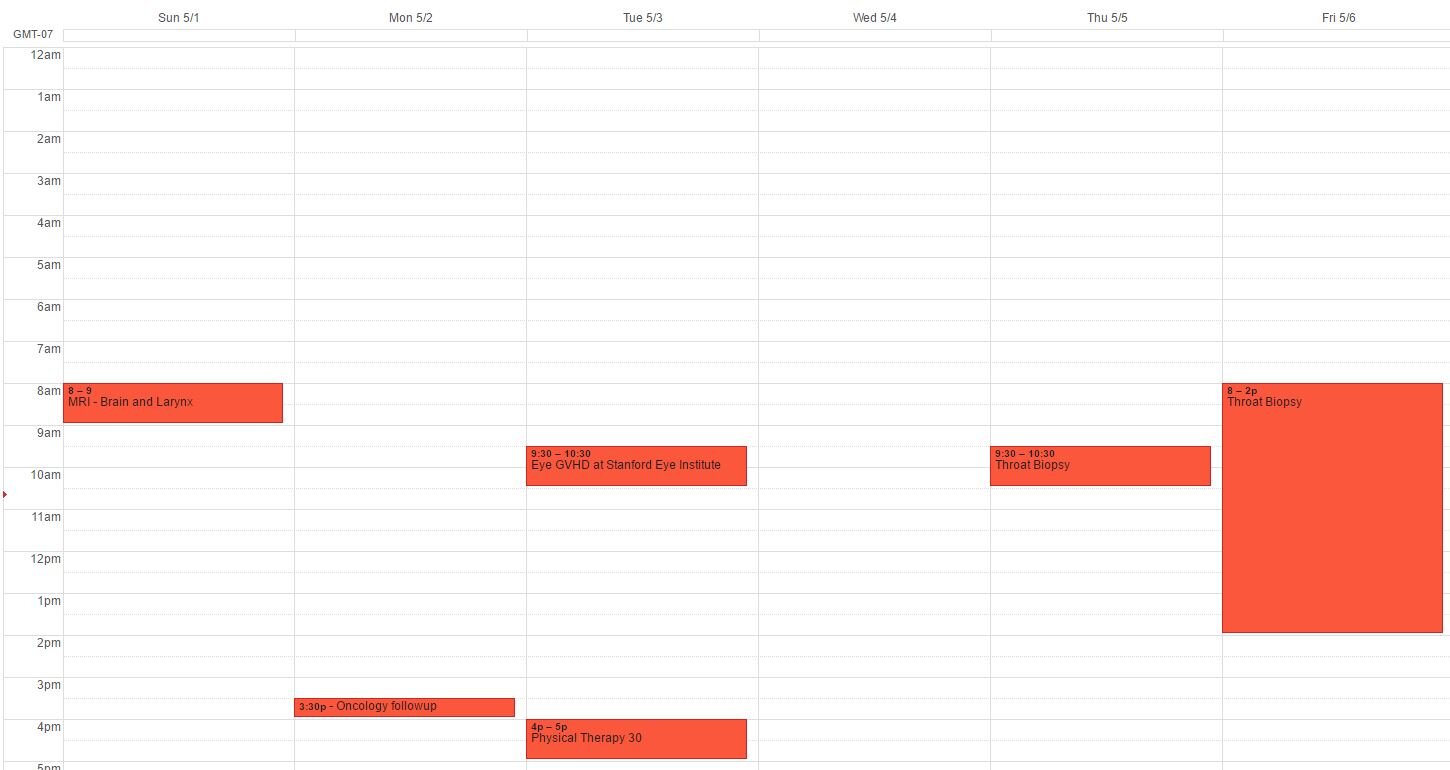
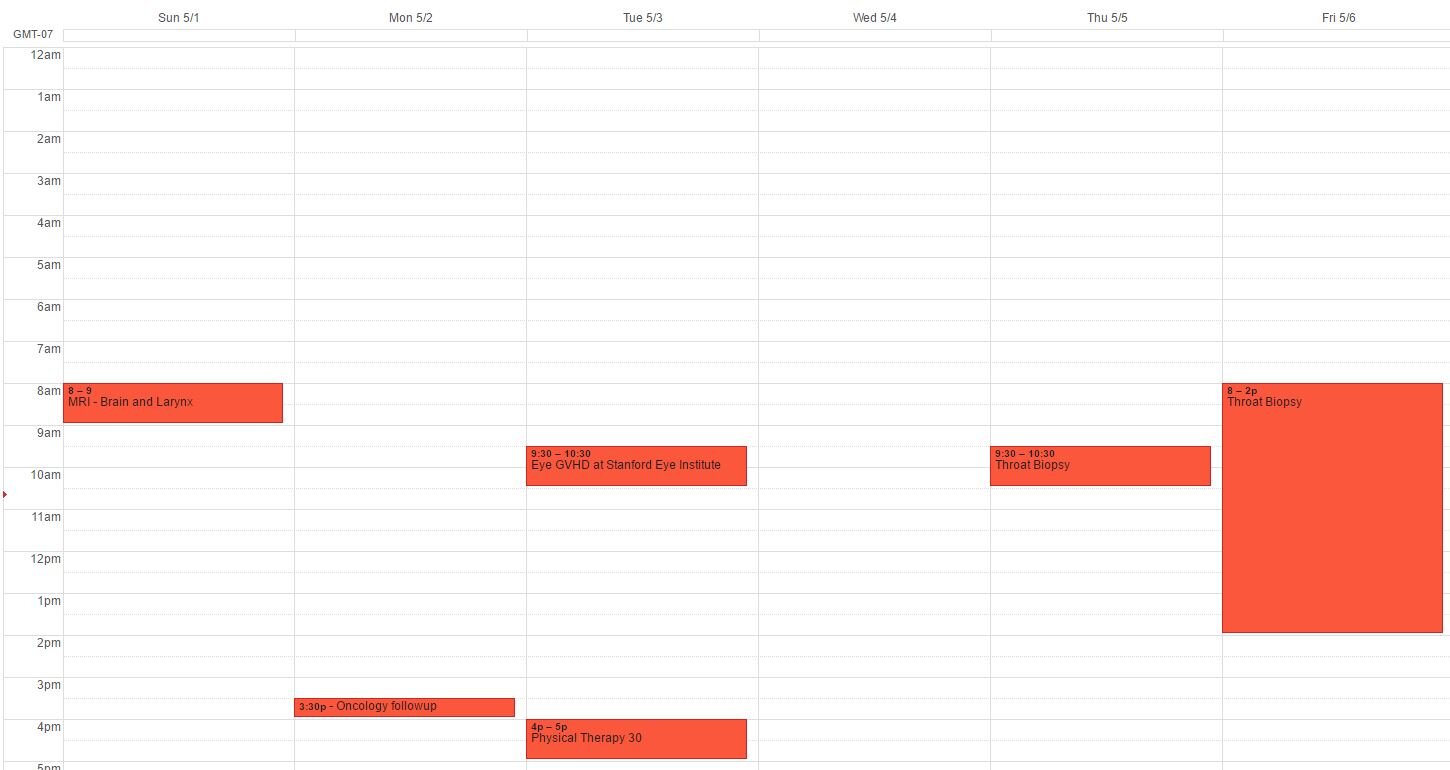
As with all cancer battles, side effect maintenance is a must. This week in Side Effects, we have a closing throat, dry eyes, sore and dry both, and peripheral neuropathy. Our various doctors and specialist appointments are usually scattered, but looking at our schedule for next week, I found that we will be at Stanford almost every day (had to clear my Wednesday for a few immobile work commitments) to comprehensively cover everything that needs to be addressed! I found this view rather interesting and wanted to share.Sunday MRI of the brain and larynx: About 8 months ago when my mom lost all her hair after chemo, she hit her head pretty hard on the edge of a table. At that time, it was painful but the pain slowly went away. Plus, we had other things to worry about, like getting rid of the cancer. Then recently, the head pain returned. We don't know if it is related to the small trauma, or something else (like the repeated chemo in her spine or delayed side effects). After several visits to the oncologist and PCP and persistent pain, we all decided an MRI would be best. Then while there, since she also is experiencing breathing problems (had to take a trip to the ER at one point, but that's for another post), we added on an MRI of the larynx. We think her throat is operating at 50% capacity due to some build up (maybe protein) of sorts. What this means is that the moment she has a cold or slight allergies, her throat basically closes up making it hard or almost impossible to breathe. For most of us, having some allergies or phlegm in our throats are no big deal since the throat has the capacity to handle it.Monday Routine monthly oncology visit and labs: We see our bone marrow specialist once a month to check blood counts, overall health, and progression of Graft vs. Host disease. This usually means a quick health check, making sure blood counts are good, and adjusting medications (like prednisone and tacrolimus) as needed. And if we have time, a free added chair massage courtesy of Stanford Cancer Center!Tuesday morning Eye Doctor and afternoon Physical Therapy: Both these visits are to manage side effects of the chemotherapy, radiation, and donor lymphocyte infusion (DLI). The DLI has cause graft vs. host disease in the eyes, causing them to be very dry and producing almost zero tears. The ophthalmologist has put in tear duct plugs to try to retain whatever tears her eyes do make, hoping that one day the tears will return. We see him about every 6 weeks to check in. The physical therapy appointment is in response to the peripheral neuropathy and weakness caused by the chemotherapy (most likely the vincristine). My mom loves her physical therapist Shannon, and both the strengthening exercises as well as the conversations they have help improve her health. She used to not be able to get up out of a chair or close the trunk of a car. Now she can do all those things.Wednesday break day!Thursday pre-op visit for the throat biopsy: Last Monday, we went to the ER because my mom couldn't breath. Her throat had almost closed up entirely. With a camera in the throat, we discovered that some build up has been causing the throat to operation at about 1/2 capacity, making air intake harder. Her oxygen levels come back at 100% and her lungs are clear (Xray and listening), so we will do a biopsy to see what the build-up might be, and if there is a way to manage it. One of the ENT doctors think it might be Amyloidosis of the throat, but that is usually only seen in AML patients, not ALL (What my mom had). The oncologist and I are skeptical of the amyloidosis diagnosis, but we all agreed that a biopsy of the throat, taking about a 1-2mm sample, will help us decide.Friday biopsy day!One question I always ask at every step is What are the side effects of these procedures. If the MRI and biopsy will cause other complications, we need to know so we can make informed decisions about whether or not to proceed. We've been told that the side effects at trivial and the danger of not finding out the cause of some of these problems may be worse. It is always a trade-off of waiting to see if the body will take care of itself, or if we need to intervene is some other way. In this case, we shall proceed with more modern medicine interventions.