As with all cancer battles, side effect maintenance is a must. This week in Side Effects, we have a closing throat, dry eyes, sore and dry both, and peripheral neuropathy. Our various doctors and specialist appointments are usually scattered, but looking at our schedule for next week, I found that we will be at Stanford almost every day (had to clear my Wednesday for a few immobile work commitments) to comprehensively cover everything that needs to be addressed! I found this view rather interesting and wanted to share.Sunday MRI of the brain and larynx: About 8 months ago when my mom lost all her hair after chemo, she hit her head pretty hard on the edge of a table. At that time, it was painful but the pain slowly went away. Plus, we had other things to worry about, like getting rid of the cancer. Then recently, the head pain returned. We don't know if it is related to the small trauma, or something else (like the repeated chemo in her spine or delayed side effects). After several visits to the oncologist and PCP and persistent pain, we all decided an MRI would be best. Then while there, since she also is experiencing breathing problems (had to take a trip to the ER at one point, but that's for another post), we added on an MRI of the larynx. We think her throat is operating at 50% capacity due to some build up (maybe protein) of sorts. What this means is that the moment she has a cold or slight allergies, her throat basically closes up making it hard or almost impossible to breathe. For most of us, having some allergies or phlegm in our throats are no big deal since the throat has the capacity to handle it.Monday Routine monthly oncology visit and labs: We see our bone marrow specialist once a month to check blood counts, overall health, and progression of Graft vs. Host disease. This usually means a quick health check, making sure blood counts are good, and adjusting medications (like prednisone and tacrolimus) as needed. And if we have time, a free added chair massage courtesy of Stanford Cancer Center!Tuesday morning Eye Doctor and afternoon Physical Therapy: Both these visits are to manage side effects of the chemotherapy, radiation, and donor lymphocyte infusion (DLI). The DLI has cause graft vs. host disease in the eyes, causing them to be very dry and producing almost zero tears. The ophthalmologist has put in tear duct plugs to try to retain whatever tears her eyes do make, hoping that one day the tears will return. We see him about every 6 weeks to check in. The physical therapy appointment is in response to the peripheral neuropathy and weakness caused by the chemotherapy (most likely the vincristine). My mom loves her physical therapist Shannon, and both the strengthening exercises as well as the conversations they have help improve her health. She used to not be able to get up out of a chair or close the trunk of a car. Now she can do all those things.Wednesday break day!Thursday pre-op visit for the throat biopsy: Last Monday, we went to the ER because my mom couldn't breath. Her throat had almost closed up entirely. With a camera in the throat, we discovered that some build up has been causing the throat to operation at about 1/2 capacity, making air intake harder. Her oxygen levels come back at 100% and her lungs are clear (Xray and listening), so we will do a biopsy to see what the build-up might be, and if there is a way to manage it. One of the ENT doctors think it might be Amyloidosis of the throat, but that is usually only seen in AML patients, not ALL (What my mom had). The oncologist and I are skeptical of the amyloidosis diagnosis, but we all agreed that a biopsy of the throat, taking about a 1-2mm sample, will help us decide.Friday biopsy day!One question I always ask at every step is What are the side effects of these procedures. If the MRI and biopsy will cause other complications, we need to know so we can make informed decisions about whether or not to proceed. We've been told that the side effects at trivial and the danger of not finding out the cause of some of these problems may be worse. It is always a trade-off of waiting to see if the body will take care of itself, or if we need to intervene is some other way. In this case, we shall proceed with more modern medicine interventions.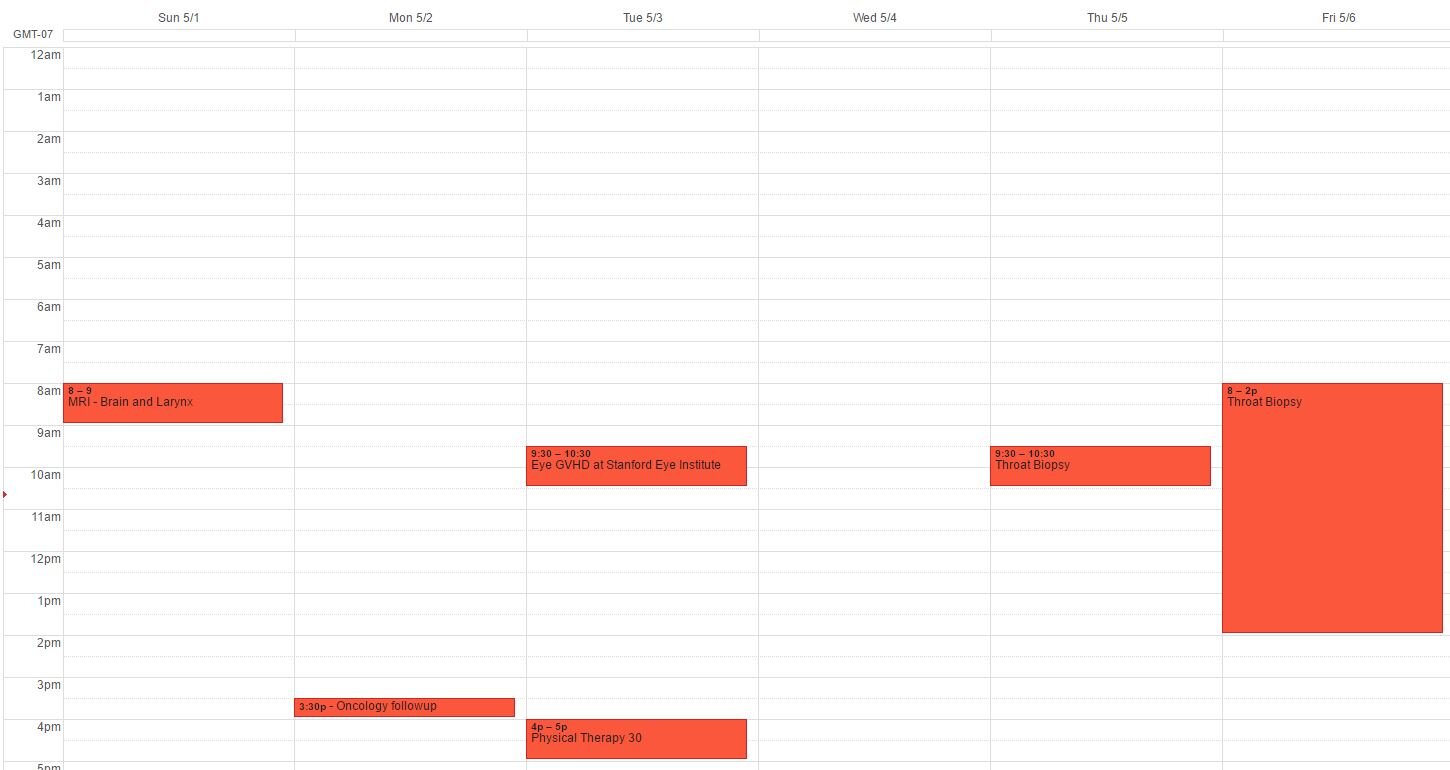
Neupogen
Neupogen is a drug used to stimulate the development of white blood cells (WBC). Chemotherapy patients are often given this shot in the stomach to help the WBCs regenerate. Although that sounds peachy, I always have been a bit skeptical about using a drug to mess with the chemotherapy and artificially cause the bone morrow to produce more white blood cells. However, when doctors tell you that you need it because the WBC count is so low that deadly infections can happen, you agree. However, a few days into it, I realized a few items:
- Not all doctors prescribe Neupogen. When I pushed back on Neupogen, eventually some doctors indicated it was optional, which leads me to the wonder why doctors just give patients such a strong shot without really discussing it in the first place. Giving hospital inpatients drugs without really discussing impact and need is another issue.
- When a nurse found out we had a biopsy scheduled in a few days, she told us to stop Neupogen immediately because it can cause an artificial count of cancer cells (blasts). No one mentioned this previously, but all the Nurse Practitioners and Physicians Assistants at Stanford agreed that we should stop Neupogen several days prior to a bone marrow biopsy.
I know that Neuopgen is prescribed so neutropenic (low white blood cell) patients do not get sick. However, it is always critical to know why it is given, and if it makes sense My continued lesson here is that the need to have patient advocate or be your own patient advocate is so high. Nurses and doctors, no matter now brilliant, do not always have the full picture of each individual's treatment plan, so we need to tell them.
CNS Prophylaxis #5!
I have a backlog of posts about CNS prophylaxis side effects, kidney stones, a nephrolithotomy, and hospital staff. Hopefully I will get around to those soon!Today is Mama Pham's fifth CNS Prophylaxis. I have written about this procedure in the past. It is chemo that is inserted into the spine as preventative measure. Leukemia cells can infiltrate the Central Nervous System, but normal chemo cannot. Therefore, oncologists take preventative measures and insert chemo directly into the spine. While doing so, they first draw some spinal fluid to test for irregularity. The process of puncturing the spinal tissue and drawing fluid often causes patients to get extreme headaches because of the depletion of fluids around the brain. This can be remedied with drinking fluids or getting fluids through IV. However, if there is a leak at the puncture point, spinal fluid continues to leak into the body, causing continuous fluid depletion around the brain. That causes continuous headaches, nausea, dizziness and neck pain that cannot be remedied by much, not even strong pain medications. The leak is caused by the body's inability to quickly heal the wound.She has had very different reactions to the past four procedures. Here's to a successful, pain-free, headache and nausea free Lumbar Puncture!
Biopsy results! No evidence of Leukemia!
Mama Pham's 100 Days Post-Transplant Biopsy came back clear! There are no Leukemia cells present. She is currently cancer-free!She has dropped to 92lbs and is still taking about 12-14 meds per day, but we are definitely one huge leap closer to full remission. She is not considered to be in full remission until the 2 year mark. 110 Days Down. 630 Days to go!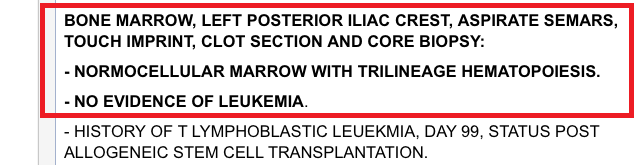
"Your medication is not covered."
We have had numerous calls from the pharmacy telling us that some medication is not covered by insurance. They said that if the doctor can verify that the patient really needs the medication then the insurance will cover it. One call to the doctors' office usually does the trick. My question then is this:
How often do doctors prescribe medications that patients do not actually need?
Day 16! Cancer Free Peripheral Blood! WBC Count of 3.0!
Much has happened in the last 16 days! As you may recall from a previous post, the stem cell transplant day is Day Zero. We are now on Day 16. The first two weeks are the hardest part of any stem cell transplant. The patient feels all the side effects of the radiation and chemotherapy from the previous week and the body has to deal with having 8.7 million new cells from another person's body. Here's now I like to compare it to a wartime scenario: The original fort (the body) is almost completely annihilated with different types of poison (radiation and chemo in this case) leaving just enough infrastructure so that the fort can be rebuilt. Once it is deemed that enough of the enemy has been eradicated, a completely new army (enemy/cancer free) is sent in to rebuild. The fort is still reeling from all the damage, and the army still has not adjusted so the first two weeks is quite rough. Hopefully, soon, all the damage slowly starts to heel, the army gets acclimated and everything works in full force to rebuilt the fort again. During that time, we just hope that no other enemy comes in to attack since neither the fort nor the army are ready for battle!During the past two weeks, unfortunately, my mom's defenseless body has had to fight some infections. She has had bronchitis in both lungs, swollen intestines and many mouth and throat sores from the radiation and chemotherapy. The hospital has kept those infections under control by varying different anti-fungal and antibacterial medications. She has been put on oxygen several times to help her breathing. She was also put on Total Parenteral Nutrition (TPN), which is food through the IV since she has been unable to eat. She has been hanging in there.Yesterday, we heard great news. Her peripheral blood is completely cancer free and her WBC is up to 3.0! We still need to wait on bone marrow biopsy to see if my uncle's stem cells have grafted and if the bone marrow is cancer free. She has always had disease in the bone marrow and not just the peripheral blood. But this news is great news so far. There is still much ahead, but this is fantastic news at this point. Next week, we will have more scans to figure out the source of some of her infections, have a bone marrow biopsy done at one point and hopefully get her eating real food again. :)Here are some references from medical resources that have some nice summaries about stem cell transplants and the donation process:http://medicine.utah.edu/internalmedicine/hematology/bloodMarrow/collection.htmhttp://www.cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/bonemarrowandperipheralbloodstemcelltransplant/stem-cell-transplant-transplant-process
Rest Day!
Since admission day on January 19th, 2014, Mama Pham has had radiation treatments twice a day. Usually around 8am, then back again at 2pm. She hated all 10 of those Intensity Modulated Radiation Therapy appointments. Her last radiation visit was Friday afternoon. On Saturday, they gave her a dose of Etoposide, an anticancer drug with rough side effects. But today is rest day! It falls on a Sunday, on the 7th day of treatment.Her appetite quickly diminishing, partly due to the side effects and partly due to the fact that she doesn't like the hospital food. City of Hope has a fairly decent hospital menu, but since the food isn't typically Vietnamese, my mom has a hard time eating it. Outside food is not allowed unless the patient eats it within one hour of preparation. I have spoken to her doctors and dietician and at one point if she continues eating very little, she may have to put on IV food.Upcoming important dates:January 28th: Mama Pham's Birthday!January 29th: My uncle's stem cells get harvestedJanuary 30th: Transplant Day
Drug Interaction - 2013 Style
My mom recently developed a blister at the location of the PICC line dressing. The nurse on call mentioned she may want to take Benadryl to help with what she believes to be an allergic reaction to the dressing. Since she was not sure if Benadryl would interact with any of my mom's current drugs, she told me to call her pharmacist. While on call with the pharmacist, I decided to just do a quick Google search for drug interactions, since this is a problem that can easily be solved with a database. The internet comes through once again! Thanks Medscape. Before the CVS pharmacist came back on the line, I already had my answer about Benadryl. I wonder if she used a similar site to look up the information she recited to me over the phone. That said, I did not know about the other interactions! Neither the doctor nor the pharmacy warned us about these other problems with an increase in OTc intervals.http://reference.medscape.com/drug-interactionchecker
Day 11 of Chemo: Last does of Vincristine!
Today, my mom receives her last dose of chemotherapy for this first cycle. We are on Day 11 and the drug is called Vincristine (brand name = Oncovin). It is given intravenously through her picc (peripherally inserted central catheter) line. Her Complete Blood Counts (CBC) are as follow:
- White Blood Cells: 0.3, severe neutropenic, high risk of infection. Normal is 5.0-10.0 in healthy adults.
- Hemoglobin: 9.2, no need for transfusion! Normal is at least 12 for women.
- Platelets: 58. Normal is 150-400. Concerning is below 20. She is low, but not at the concerning level.
The WBC count is what we are watching the most. It needs to get above 5 for the doctor to let her get on the plane and above 2 for me to stop worrying about random visitors! More about neutropenia and white blood cell counts here.Here's to a restful night.
Leukine, you troublemaker
This morning, during Dr. Lewis' daily checks, he informed us that he found some blasts in her blood smear. Blasts are immature white blood cells that should not be found in the circulating blood. He mentioned this might be due to the Leukine injections in her stomach, which assist with the production of white blood cells to help maintain a level that can better fight infection. I previously wrote about Leukine here. Since the Leukine might be causing problems with blasts, he has stopped the Leukine injections. For us, this means we will need to continue to be fastidious about what she eats, who she sees and what she touches so she does not get sick.
This means not allowing just anyone to visit. Yesterday, one of her previous co-workers decided to stop by and despite all of her objections, brought a bag of overly-ripe bananas and home-made cold foods. Ain't nobody got time for that.
Leukine and White Blood Cell (WBC) Counts
My mom came to St. Joseph's Hospital on Friday, August 10th with a crazy high white blood cell count of 90.0 x 10^9 WBCs/liter. Normal amounts for men and non-pregnant women women ranges from 4.5 - 10.0 x 10^9 WBCs/liter. After transfusions and treatment, they were able to bring the WBC count down to normal levels. As her chemotherapy hyper-CVAD drugs take effect, her WBC count has slowly dropped. Right now, it is at 1.2 x 10^9 WBCs/liter. She is classified as neutropenic and put on a neutropenic diet where she avoids anything fresh that can potentially bring increase infection. During this period, it is critical that she does not get sick since it is more difficult for her body to ward off infection with such a low WBC count. She has already had most of her chemo drugs for this first cycle of hyper-CVAD and now is the waiting period for the drug to wipe out the bad WBCs and wait for the body to rebuild the good WBCs. To help with rebuilding, Dr. Lewis has prescribed injections of Leukine into the stomach.Leukine is the trade name for Sargramostim. According to Wikipedia recombinant granulocyte macrophage colony-stimulating factor (GM-CSF) that functions as an immunostimulator. Yes. Let's try the description from Leukine.com:Leukine is used to help the number and function of white blood cells after bone marrow transplantation, in cases of bone marrow transplantation failure or engraftment delay, before and after peripheral blood stem cell transplantation, and following induction chemotherapy in older patients...Basically, it is a drug to help the little white blood cell army rebuild its force.